Hyperpigmentation: Causes, Types, and Modern Treatment Methods

Introduction
Hyperpigmentation is one of the most common skin problems affecting people of all ages. Dark spots on the skin can appear due to sun exposure, hormonal changes, skin trauma, or improper skincare. Although this condition is not dangerous to health, it often causes aesthetic discomfort and can affect self-confidence. In this article, we will discuss what hyperpigmentation is, its causes, types, and modern treatment methods that help address this issue.
What is Hyperpigmentation?
Hyperpigmentation is a skin condition where an excess of melanin (the skin’s natural pigment) accumulates in certain areas. This results in darker spots or patches that may vary in size and shape.
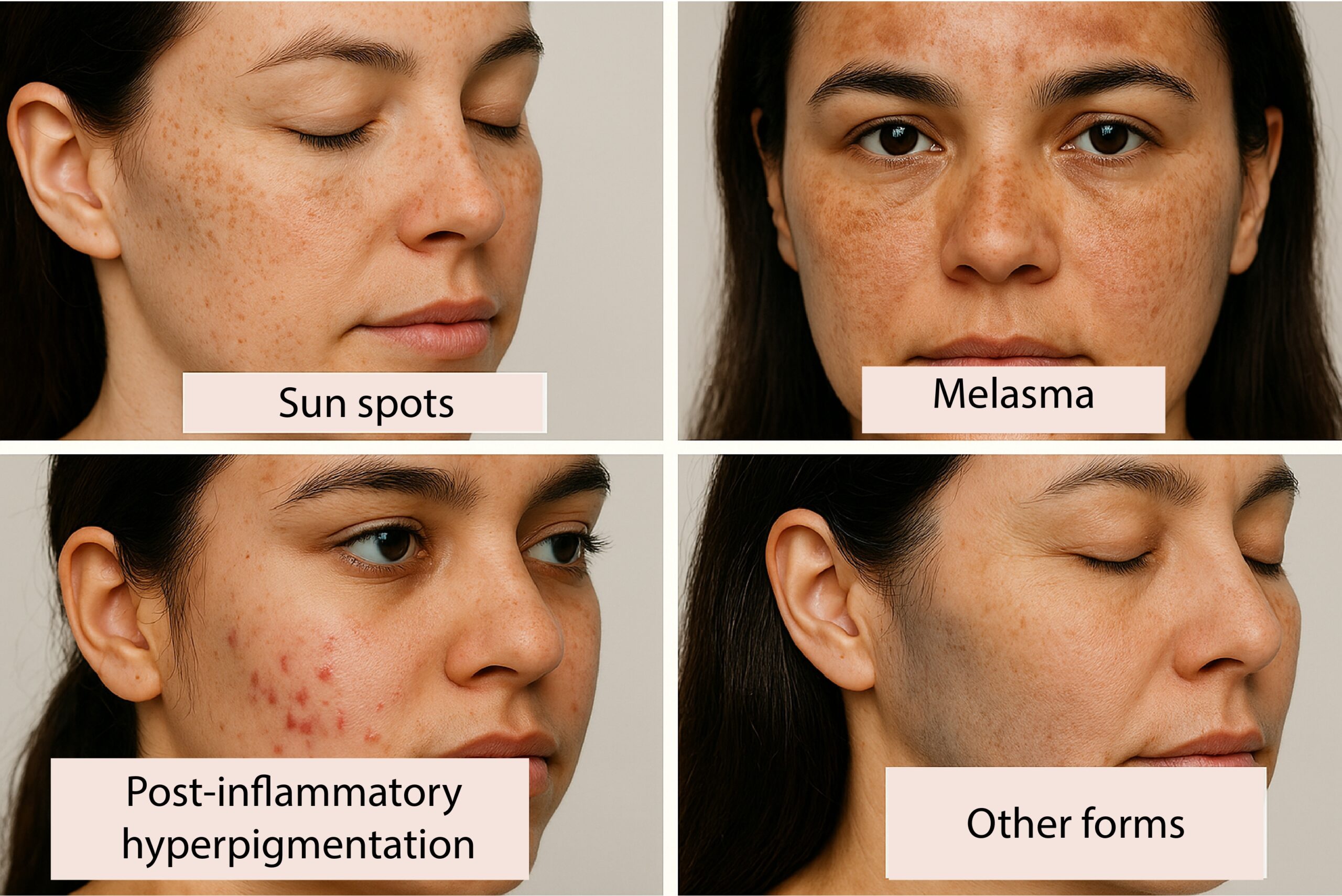
Types of Hyperpigmentation
1. Sun spots (lentigo, solar lentigines): usually appear in older age due to long-term sun exposure.
2. Melasma: irregularly shaped patches, typically on the face, often linked to hormonal changes (pregnancy, contraceptives).
3. Post-inflammatory hyperpigmentation: occurs after skin inflammation or trauma, such as acne, scratches, or aggressive cosmetic procedures.
4. Other forms: caused by genetic factors, certain medications, or chronic skin conditions.
Causes and Risk Factors
-
Sun UV rays – the main trigger for melanin production
-
Hormonal changes – pregnancy, menopause, use of contraceptive pills
-
Skin inflammation and trauma – acne, cuts, dermatological procedures
-
Genetic predisposition
-
Certain medications (e.g., photosensitizing drugs)
Symptoms
- Dark spots or patches, usually on the face, hands, or chest
- Spots may appear brown, grayish, or even black
- Unchanged skin texture
- Usually no itching or pain
If spots change in shape, size, or color, or are accompanied by symptoms such as itching, bleeding, or inflammation, you should see a dermatologist as soon as possible. These may be signs of other skin conditions, not just hyperpigmentation, and early testing is essential.
When to See a Doctor?
- If spots appear suddenly, grow quickly, or change in shape
- If hyperpigmentation causes emotional distress
- If spots are accompanied by other symptoms (itching, bleeding, inflammation)
Diagnosis
A dermatologist diagnoses hyperpigmentation by:
- Visually examining the nature of the spots
- Using dermatoscopy (a special tool to view skin structures)
- If necessary, performing additional tests such as a skin biopsy to rule out other diseases (e.g., skin cancer)
Treatment Options
Daily skincare:
- Use sunscreen with SPF 50+
- Gentle cleansing and moisturizing
Active ingredients in topical products:
- It’s important to note that while ingredients like vitamin C, niacinamide, fruit acids (AHA, BHA), and retinoids can help improve skin condition, they should be tailored to individual skin types. Not all products are suitable for everyone, so it’s recommended to consult a dermatologist before using such products to ensure safe and effective application.
• Stronger treatments should be used only under a dermatologist’s supervision — their use depends on individual cases.
Dermatological procedures:
- Chemical peels
- Laser treatment (e.g., fractional laser)
- Microneedling therapy
- Mesotherapy with brightening agents
It’s important to emphasize that stronger treatments like chemical peels, laser therapy, and other dermatological procedures should be performed only under the supervision of a qualified dermatologist. These treatments may cause side effects such as irritation, inflammation, temporary redness, or peeling. Laser therapy may be unsuitable for certain skin types (e.g., darker skin tones), as it can lead to hypopigmentation or other complications. Always consult a specialist before beginning treatment to ensure the most appropriate plan for your skin condition.
Care and Prevention
- Use broad-spectrum sunscreen daily
- Avoid aggressive skin treatments without professional supervision
- Monitor skin condition after inflammation or acne
- Choose gentle skincare products
Frequently Asked Questions (FAQ)
Can hyperpigmentation fade on its own? Some forms (especially post-inflammatory hyperpigmentation) may fade over time, but treatment is often needed.
Is hyperpigmentation dangerous to health? In most cases – no. However, any sudden changes in skin should be examined by a doctor.
How long does treatment take? It depends on the type, depth of pigmentation, and chosen treatment method. Results may be visible in a few weeks or months, but some spots fade gradually and others may require long-term treatment.
Conclusion
Pigmentation spots are a common but manageable skin issue. Although many treatments are available, it’s important to understand that not all solutions work for everyone. Effective treatment depends on the cause, skin type, and overall condition.
Choosing skincare products on your own may not only be ineffective but could worsen the condition. Therefore, consulting with a specialist is essential to find the most suitable treatment method tailored to your individual needs.
💬 Have concerns or noticed changes in pigmentation? Contact iDerma specialists — we’ll help you resolve the issue safely, professionally, and personally.


1. Oge’ LK, Broussard A, Marshall MD. Acne Vulgaris: Diagnosis and Treatment. Am Fam Physician. 2019 Oct 15;100(8):475-484.
2. Eichenfield DZ, Sprague J, Eichenfield LF. Management of Acne Vulgaris: A Review. JAMA. 2021 Nov 23;326(20):2055-2067.
3.Nast A, Dréno B, Bettoli V, Bukvic M. Z, Degitz K, Dressler C, Gollnick H. European evidence‐based (S3) guideline for the treatment of acne–update 2016–short version. Journal of the European Academy of Dermatology and Venereology. 2016, 30(8), 1261-1268.
Mycosis Fungoides
The most common primary skin T-cell lymphoma (cancer of the blood). Mycosis Fungoides is characterized by three main stages, several of which may exist at the same time
Paraneoplastic dermatological manifestation of gastrointestinal malignancies
rare disorders resulting from the immune system’s response to a cancerous process (neoplasia) in the body. Gastrointestinal neoplasms more often cause paraneoplastic syndromes affecting the skin.
Nail psoriasis
Psoriasis is a form of chronic systemic inflammatory autoimmune disease that mostly affects fingernails and toenails.




