Focal alopecia

Focal alopecia (alopecia areata) is an autoimmune condition that causes hair loss. It usually manifests as localized hair loss on the scalp, but it can also occur on other hairy parts of the body.
Prevalence
The frequency of the disease is not related to race, gender, it can occur in both children and adults. However, it is more often observed in people aged 20-30 years. The overall probability of developing this disease in the course of life is about 2%.
People who are more likely to get focal alopecia:
- have other autoimmune diseases
- thyroid diseases
- have changes in the set of chromosomes (eg: Down syndrome)
- there are people with alopecia in the family (since the disease is linked to genetic inheritance)



Mechanism of injury
Hair growth is divided into phases:
- Anagen phase (active growth) lasting from one to eight years;
- Catagen phase (transformations), lasting several weeks;
- The telogen (resting) phase lasts for several months, after which it enters the exogen (shedding) phase.
The exact mechanism of hair loss is not known, but it is associated with damage to the hair in the anogen phase, when the hair does not form properly and quickly transitions to other phases.
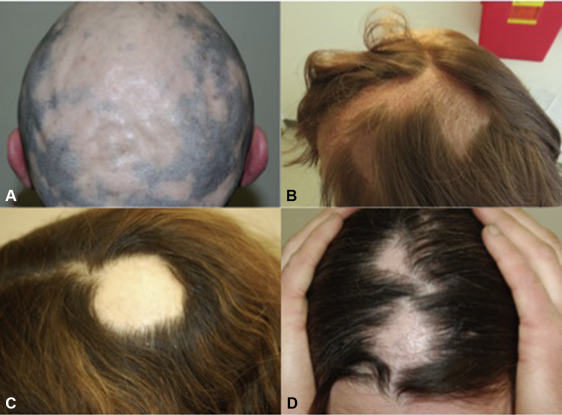
Clinical signs
Alopecia areata usually manifests as focal baldness, leaving round patches of skin in the hairy area. The scalp is most often affected, less often the beard, eyebrows, eyelashes. Some patients may experience local tingling or itching before hair loss, and about 10-40% of patients experience changes in the nails (e.g. nail indentation, deepening of furrows).
How is alopecia diagnosed?
The diagnosis is usually based on the clinical picture, additional tests may be performed if necessary:
- Trichoscopy (examination of the hair follicle, hair shaft and scalp with a dermatoscope);
- Hair extraction test (about 40-60 hairs growing next to each other are grasped, gently pulling, the test is considered positive if more than 10% of the grasped hairs are extracted);
- Skin biopsy
Treatment
For less than 50% bald areas Corticosteroid (hormone) injections, local treatment with strong corticosteroids, dithranol, minoxidil can be used for damage to the hairy area. Local immunotherapy, systemic corticosteroids, systemic JAK inhibitors in case of a larger lesion area.
It is important to familiarize the patient with the solutions to the disease, because focal alopecia is not a curable disease, it can disappear by itself, recur or progress. Therefore, it is important to inform the patient about the possibilities and effectiveness of the treatment, in case of great discomfort it is useful to recommend professional consultations that improve the emotional state, support groups that would help to come to terms with the changes in appearance.
If you do not know which method of treatment is the most suitable for you, consult a dermatovenerologist.


1. Darwin E, Hirt P, Fertig R, Doliner B, Delcanto G, Jimenez J. Alopecia areata: Review of epidemiology, clinical features, pathogenesis, and new treatment options. Int J Trichol. 2018;10(2):51. doi:10.4103/ijt.ijt_99_17.
2. Messenger AG, McKillop J, Farrant P, et al. British Association of Dermatologists’ guidelines for the management of alopecia areata 2012. British Journal of Dermatology. 2012;166(5):916–26. doi:10.1111/j.1365-2133.2012.10955.x.
3. Strazzulla LC, Wang EHC, Avila L, Lo Sicco K, Brinster N, Christiano AM, Shapiro J. Alopecia areata: Disease characteristics, clinical evaluation, and new perspectives on pathogenesis. J Am Acad Dermatol. 2018 Jan;78(1):1-12. doi: 10.1016/j.jaad.2017.04.1141. PMID: 29241771.
Nail psoriasis
Psoriasis is a form of chronic systemic inflammatory autoimmune disease that mostly affects fingernails and toenails.
Lyme disease
It is contracted when a blood-sucking tick injects intestinal contents containing bacteria into a wound. Untreated Lyme disease can damage not only the skin, but also the internal organs, joints and nervous system.
Psoriasis
A common, chronic, inflammatory, recurring skin disease that affects 2-3% of the population. Psoriasis can start at any age, and is most often found in adults.
iDerma
MB iDerma
Fabijoniškių g. 99, Vilnius
+370 670 70822
info@iderma.lt




